Introduction: Chronic Graft-versus-Host Disease (cGvHD) frequently requires prolonged immune suppressive therapy (IST) with > 50% still on IST at 5 years. The IST typically involves a slow taper of steroids often with flare of cGvHD, necessitating augmentation of previous therapy or addition of new IST. Studies describing cGvHD flares are limited. We analyzed patients with cGvHD who flared during the treatment with systemic IST, their overall survival (OS) and non-relapse mortality (NRM).
Methods: This study included all adult patients with cGvHD (n=145) following an allogeneic transplant (2010 - 2017) from a matched sibling donor peripheral blood stem cell transplant (MSD, n=104 (72%) or double/single umbilical cord blood transplant (UCBT, n=41 (28%). The 2014 NIH Consensus Criteria were used to classify organ/overall cGvHD severity. Flare of cGvHD was defined as progression in cGvHD manifestations (after initial response), which was less severe than at diagnosis. Multivariate regression of flares was based on the Prentice, Williams and Peterson model for ordered multiple events (flares). Time-dependent effects on OS and NRM were analyzed by Cox and Fine and Gray regression with propensity scoring to control for confounding.
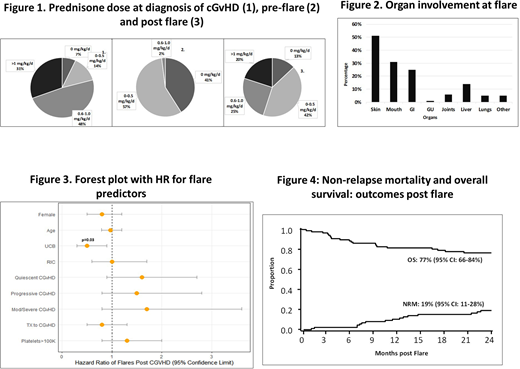
Results: Flares occurred in 87 patients; the cumulative incidence of flares was 60% (95% CI: 51-70%) at a median of 188 days (range 16-751) after diagnosis of cGvHD. The median dose of prednisone was 1 mg/kg/day (range 0-4.2) at diagnosis of cGvHD. At the diagnosis of flare, 36 (41%) of the patients were off prednisone, 50 (57%) were receiving 0.1-0.5 mg/kg /day, and 2 patients > 0.5 mg/kg /day. Thirty two of the 87 (36%) patients experienced multiple flares (2 to 4).
The most common organs involved at cGvHD flare were skin (n=45; 51%), mouth (n=27; 31%), GI tract (n=22; 25%) and liver (n=12; 14%); often in combinations of skin/mouth in 11 cases (13%), skin/GI in 6 (7%) and liver/mouth in 4 (5%) cases.
Treatment for flare was mostly increase in dose of prednisone to 0.5 mg/kg/day (range 0.3-1.0) in 77 patients (88%) plus the addition of another line of IST in 48 patients (55%).
In multiple regression analysis, only donor type was significant predictor of flare in cGvHD. UCBT was associated with 2-fold lower probability of flaring (HR 0.5; 95% CI: 0.3-0.9; p=0.03) compared to MSD. cGvHD severity, organ involvement, platelet count at diagnosis and type of onset were not significant predictors of cGvHD flares.
At 2 years after the initial flare, the OS was 77% (95% CI: 66-84%) and NRM 19% (95% CI: 11-28%). Multiple regression analysis evaluating OS and NRM from onset of cGvHD comparing flare to non-flare were performed using flare as a time dependent variable. Compared to cGvHD patients without flare at 2 years, those with flare of cGvHD had a similar risk of NRM (HR 1.2; 95% CI: 0.2-6.1, p=0.86) and OS (HR 0.9; 95% CI: 0.4-2.3, p=0.85).
At 2 years from cGvHD onset, the cumulative incidence of resolved cGvHD (durable discontinuation of steroids for ≥ 6 consecutive months) was 31% (95% CI: 21-41%) in those who flared vs. 86% (95% CI: 75-96%) in those without flare.
Conclusions: Though cGvHD patients with flare had similar risk of NRM and OS as those without a flare, patients with flare required extended steroids, along with clinical monitoring and intensified IST. cGvHD after UCBT was associated with significantly lower risk of flaring compared to MSD. The ongoing burden of IST, risk of infection and morbidity of cGvHD is substantial and needs better approaches than chronic slow taper of steroids.
Weisdorf:Incyte: Research Funding; FATE Therapeutics: Consultancy. Wagner:Novartis: Research Funding; Rocket Pharmaceuticals, Inc.: Consultancy, Current equity holder in publicly-traded company; Magenta Therapeutics: Consultancy, Research Funding; BlueRock: Research Funding; Gadeta: Membership on an entity's Board of Directors or advisory committees. Blazar:Fate Therapeutics Inc.: Research Funding; Childrens' Cancer Research Fund: Research Funding; BlueRock Therapeutics: Research Funding; BlueRock Therapeuetic: Consultancy; Magenta Therapeutics: Consultancy; KidsFirst Fund: Research Funding; Tmunity: Other: Co-founder. MacMillan:Mesoblast: Consultancy; Angiocrine Biosciences, Inc.: Consultancy; Equillium, Inc.: Consultancy; Talaris Therapeutics, Inc: Consultancy; Fate Therapeutics, Inc.: Consultancy. Holtan:Generon: Consultancy; BMS: Consultancy; CSL Behring: Other: Clinical trial data adjudication; Incyte: Consultancy. Brunstein:AlloVir: Other: Advisory board; Gamida: Research Funding; Astex: Research Funding; Magenta: Research Funding. Betts:Patent Pending: Patents & Royalties: Dr. Betts has a pending patent WO2017058950A1: Methods of treating transplant rejection. This includes the use of JAK inhibitors. Neither he nor his institution have received payment related to claims described in the patent.. Bachanova:FATE: Research Funding; Karyopharma: Membership on an entity's Board of Directors or advisory committees; Incyte: Research Funding; Gamida Cell: Membership on an entity's Board of Directors or advisory committees, Research Funding; Kite: Membership on an entity's Board of Directors or advisory committees; BMS: Research Funding. Rashidi:Synthetic Biologics: Other: DSMC member (1 trial) and related honorarium. Arora:Fate Therapeutics: Consultancy; Kadmon: Research Funding; Pharmacyclics: Research Funding; Syndax: Research Funding.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal